Medical Coding Accuracy: A 90-Day Improvement Framework
A Comprehensive Guide for Coding Managers and Medical Directors
Executive Summary
The numbers tell a stark story: healthcare organizations lose $36 billion annually to medical coding errors [1]. The average practice generating $10 million in revenue hemorrhages up to $1.5 million each year due to coding inaccuracies [1]. Meanwhile, 11.8% of medical claims were initially denied in 2024, up from 10.2% in 2020, with many denials preventable through improved coding accuracy [2].
Yet some organizations have cracked the code. They're achieving up to 99% coding accuracy while their peers struggle to reach the 95% industry benchmark. They're seeing 30% revenue increases in just 90 days. And they're doing it without expanding headcount or implementing expensive technology overhauls.
The difference? A systematic, approach combining specialty-specific education, individualized audit feedback, and customized reference tools that transforms accuracy from a compliance checkbox into a revenue driver.
This whitepaper examines HOM's proven 3-Pillar Framework for medical coding accuracy improvement, drawing from real-world implementations that have delivered measurable outcomes, including:
- 85% → 95% accuracy improvement in 3 months.
- 30% revenue increase within 90 days.
- Up to 99% sustained accuracy rates in mature implementations.
- Specialty-specific frameworks addressing high-complexity coding challenges.
If you're a Coding Manager or Medical Director facing mounting denial rates, revenue leakage, or compliance concerns, you'll discover practical strategies that work across specialties, provider sizes, and EHR platforms.
Key Takeaways:
- Education-first framework: A 3-Pillar Method—specialty-specific workshops, individualized audit feedback, and customized reference tools—consistently outperforms technology-only approaches for sustained accuracy improvement.
- 90-day measurable results: Typical implementations achieve 85% → 95%+ coding accuracy, 30% revenue increase at the same patient volume, and improved denial rates within three months.
- Baseline to sustainability: Comprehensive audits and error pattern analysis establish the foundation; ongoing quality reviews, continuous education, and peer case review maintain results.
- Proven ROI: A $10M practice can recover $1–1.5M annually. The $50–75K 90-day program delivers 12–20x ROI without expanding headcount or long technology projects.
- Compliance and risk mitigation: Improved documentation specificity and payer-policy alignment reduce improper payments, audit exposure, and enhance financial performance.
Glossary of Key Terms
CAC (Computer-Assisted Coding): Software that uses natural language processing to suggest diagnosis and procedure codes based on clinical documentation, supporting (but not replacing) certified medical coders.
Clean Claim: A claim submitted with all required information, accurate codes, and proper documentation that can be processed without additional information requests or corrections.
Clean Claim Ratio (CCR): The percentage of claims accepted by payers on first submission without denials, rejections, or requests for additional information.
Coding Accuracy Rate: The percentage of medical codes assigned correctly according to official coding guidelines, typically measured through quality audits and benchmarked at 95% industry standard.
Denial Rate: The percentage of submitted claims rejected by payers, requiring appeal, correction, or write-off. Industry average ranges from 8-12% of total claims.
Downcoding: Assigning codes for lower-level services than documentation supports, resulting in reduced reimbursement. Often occurs due to coder uncertainty or lack of specialty-specific knowledge.
E/M (Evaluation and Management) Services: Professional services including office visits, consultations, and hospital visits, coded based on complexity, time, and medical decision-making documented.
Modifier: Two-digit code appended to CPT/HCPCS codes to indicate altered circumstances, such as bilateral procedures, multiple procedures, or distinct services performed during the same encounter.
Unbundling: Billing separately for services that should be combined under a single comprehensive code, often triggering payer edits and denials.
Upcoding: Assigning codes for higher-level services than documentation supports, creating compliance risk and potential fraud allegations.
The Current State of Coding Accuracy: Industry Challenges and Financial Impact
Current Industry Performance Gaps
When you examine medical coding accuracy across healthcare organizations, the performance gaps are massive and costly. While the industry benchmark established during the ICD-9 era remains 95% accuracy, research reveals that median coding accuracy ranges from 50-98% depending on coder experience, diagnosis type, and service complexity, with a weighted median of approximately 80% [3]. This means the typical healthcare organization operates 15 percentage points below the accuracy benchmark that determines optimal reimbursement.
Table 1: Industry Performance Gap
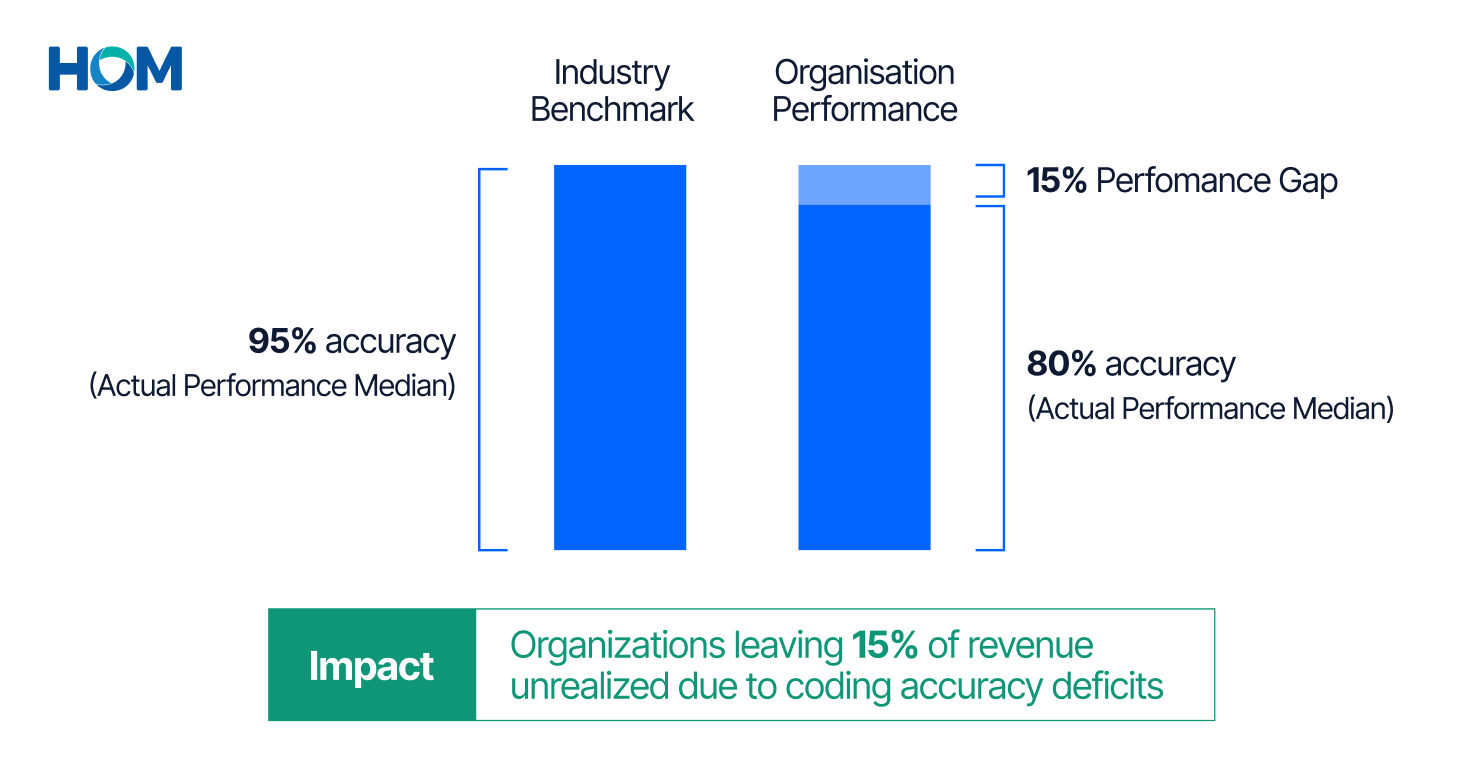
The transition to ICD-10-CM in 2016 made matters worse [4]. The expanded code specificity requirements and increased system complexity temporarily reduced accuracy rates across the industry. Many organizations never fully recovered, and the accuracy gap has persisted for nearly a decade.
Most Common Documentation Deficiencies:
- Diagnostic specificity gaps: Vague or incomplete condition descriptions that fail to support the highest level of specificity required by ICD-10-CM
- Missing chronic conditions: Failure to document chronic conditions during routine visits, particularly impacting risk adjustment programs and quality reporting
- Inadequate annual recapture: Not re-documenting previously identified conditions during each applicable encounter, creating gaps in longitudinal patient records and risk adjustment capture
- Insufficient MEAT criteria evidence: Missing documentation that conditions are Monitored, Evaluated, Assessed, and Treated, particularly problematic for chronic disease management and Medicare Advantage audits [5]
- Poor coder-physician collaboration: Communication breakdowns between clinical documentation teams and coding departments, resulting in missed opportunities for query clarification and education
- Modifier application errors: The single biggest denial driver, with missing modifiers and incorrect modifier pairing accounting for substantial claim rejections
Financial Implications of Inadequate Coding Accuracy
This isn't just about compliance metrics. The financial impact cuts deep and compounds over time.
The $36 Billion Problem:
Medical coding errors cost the US healthcare industry an estimated $36 billion annually in lost revenue, denied claims, and regulatory penalties [1]. This figure includes both undercoding (leaving money on the table) and overcoding (triggering denials and potential fraud allegations).
Government Program Impact:
- $31.70 billion (Medicare FFS): In fiscal year 2024, Medicare fee-for-service improper payments totaled approximately $31.70 billion (representing a 7.66% improper payment rate) [6]
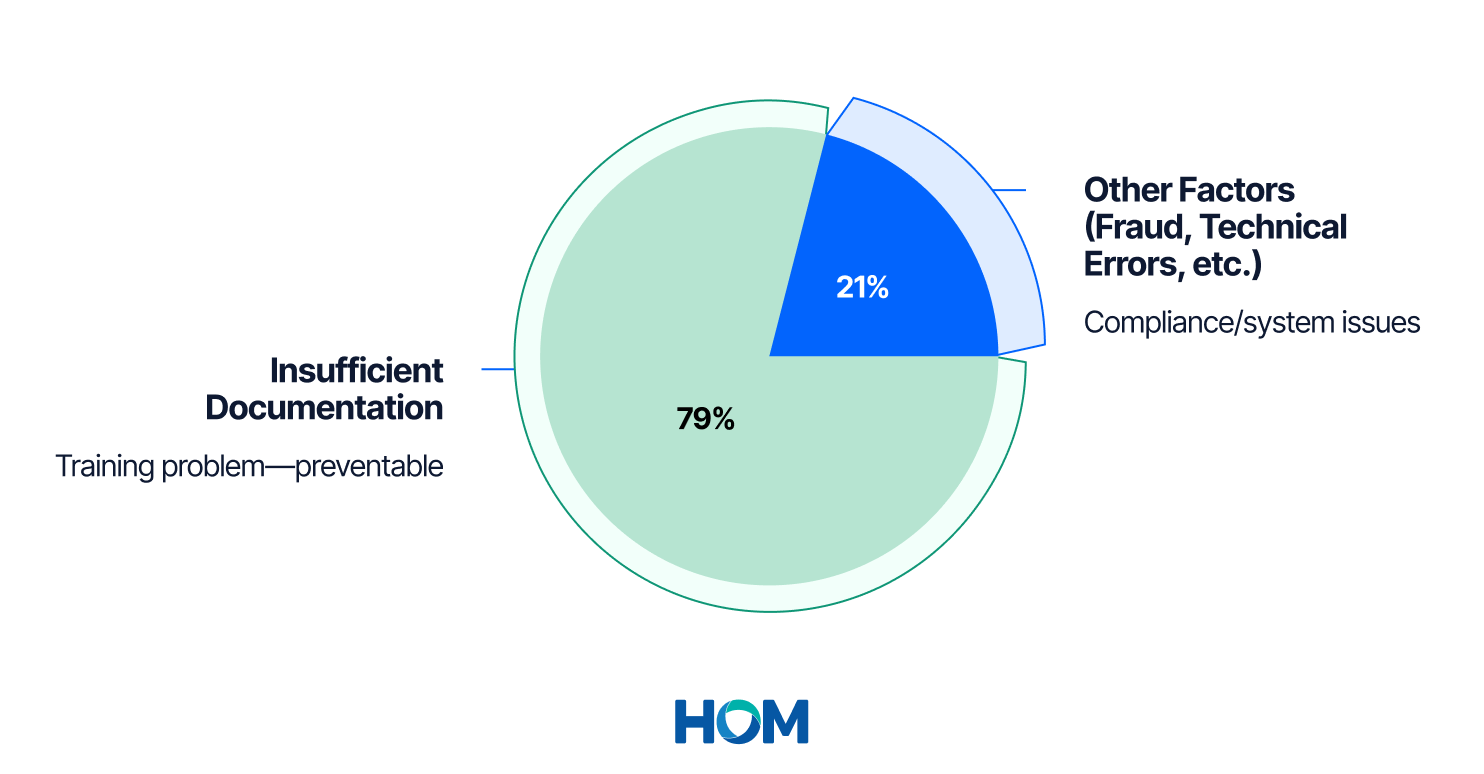
- $31.10 billion (Medicaid): Medicaid's improper payment rate of 5.09% translated to $31.10 billion in federal funds, with 79.11% of improper payments resulting from insufficient documentation rather than intentional fraud [6]
Denial Rate Economics:
- 8-12% initial denial rates: Industry analysts estimate that 8-12% of all healthcare claims are initially denied, with more than 60% potentially preventable through better documentation and coding [2]
- 25-30% of denials are coding-related: Coding denials account for approximately one-quarter of total claim denials but have significantly higher appeal overturn rates (approximately 65%) [2]
- $500-2,500 cost per denied claim: Average recovery and appeal costs vary by payer and complexity, but the administrative burden of reworking denied claims adds substantially to the total cost of poor coding accuracy
Practice-Level Revenue Loss:
The numbers get personal when you examine individual practice impact:
- $125,000 annually (small-medium practices): Small to medium-sized clinics experience revenue losses of 10-30% due to coding inaccuracies, translating to approximately $125,000 annually for many providers [1]
- $1-1.5 million annually (per $10M practice): For practices generating $10 million annually, cumulative revenue leakage from 10-15% coding error rates can reach $1-1.5 million [1]
- 12% of claims contain errors: The American Medical Association estimates that approximately 12% of claims submitted contain coding errors that impact reimbursement [2]
Table 2: Practice-Level Financial Impact Analysis: Revenue Recovery Potential (Example: $10M Annual Practice)
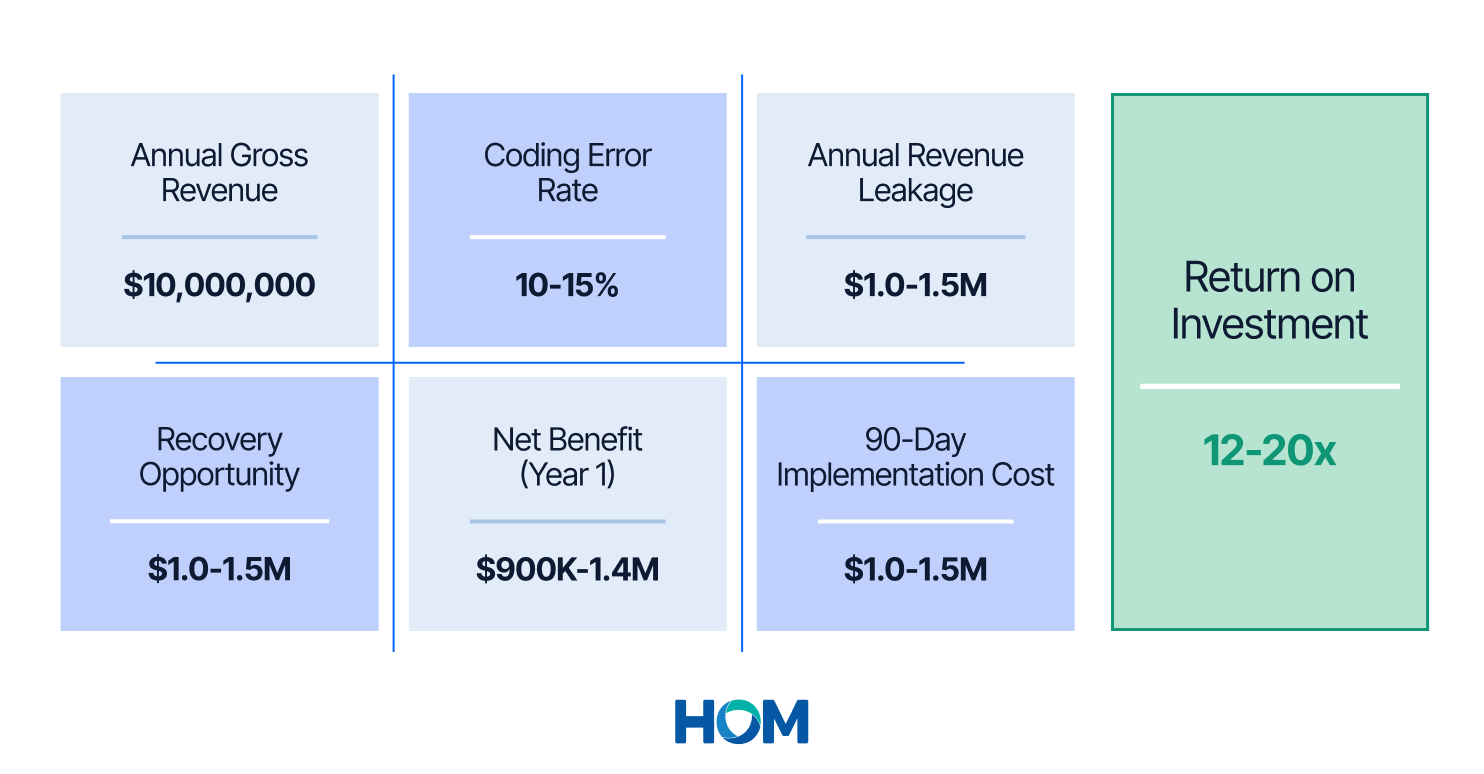
* Implementation investment depends on factors including practice size (number of providers and coders), baseline audit scope, specialty-specific requirements, and existing system infrastructure. Contact HOM for detailed pricing tailored to your organization.
Specialties at Highest Financial Risk
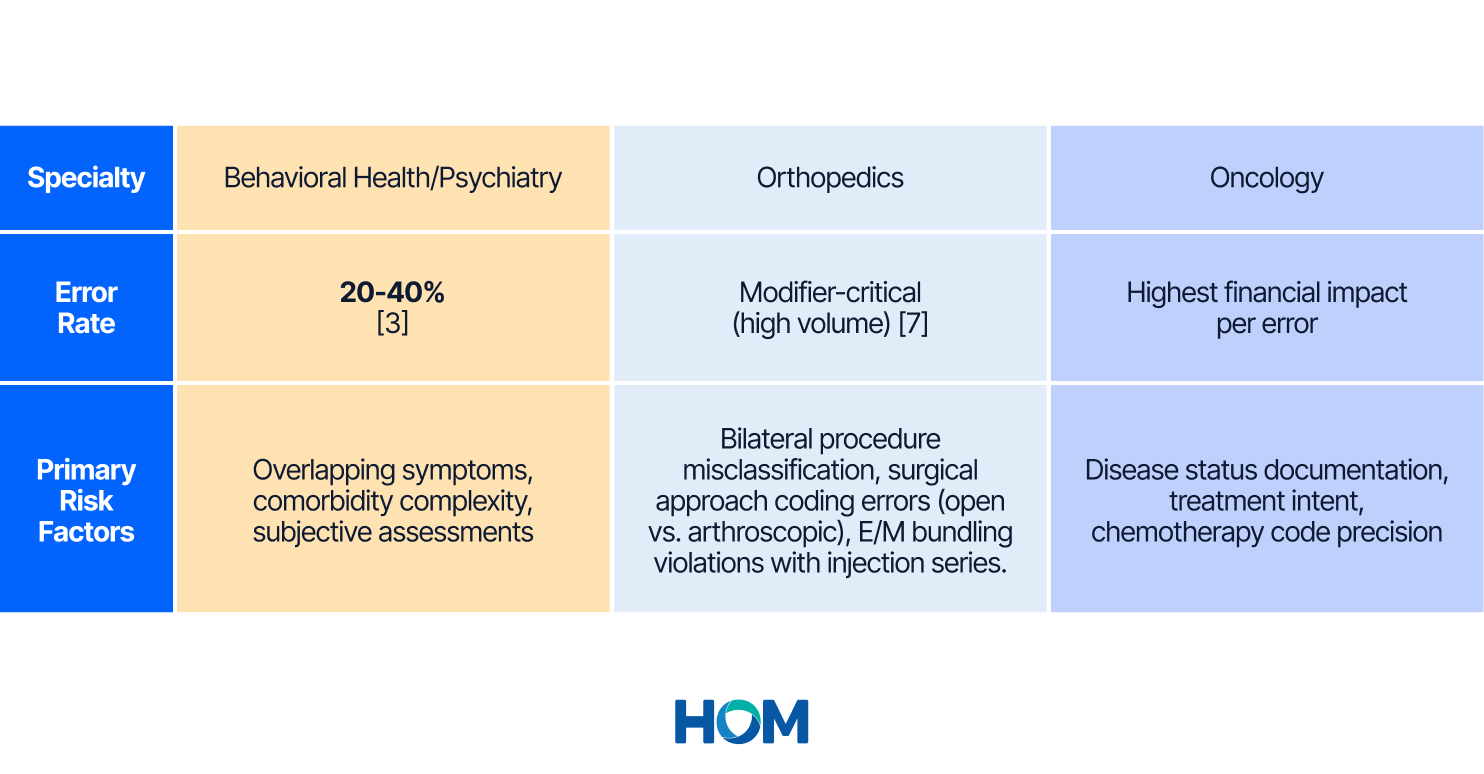
Certain specialties face disproportionate coding accuracy challenges due to service complexity, documentation requirements, and payer scrutiny:
Behavioral Health/Psychiatry: Mental health ICD-10 codes show 20-40% error rates, significantly higher than general medical coding, due to overlapping symptoms, comorbidity complexity, and subjective clinical assessments [3]. The recent 17% increase in behavioral health denial rates reflects insufficient training in specialty-specific coding requirements.
Orthopedics: High procedure volumes (orthopedic coders average 94 surgical encounters per day) combined with complex modifier requirements create substantial risk [7]. Common errors include bilateral procedure misclassification, open vs. arthroscopic procedure coding, and E/M bundling with injection series.
Oncology: The highest-complexity specialty involves expensive procedures where single coding errors result in substantial financial impact. In 2024 alone, hematologists-oncologists logged nearly $42 million in improper payments, with individual claims averaging $2,500 in losses per coding error [8]. Disease status documentation (active cancer vs. remission codes), treatment intent specification, and chemotherapy code selection require precise documentation alignment that many organizations struggle to achieve.
Table 3: Specialty-Specific Error Rates & Risk Factors
Understanding the Root Causes: Why Coding Accuracy Suffers
The Talent Crisis
The medical coding workforce faces unprecedented challenges that directly impact accuracy:
12% Talent Gap: In 2025, the American Academy of Professional Coders (AAPC) estimates a 12% talent gap in medical coding across the United States [9]. Demand for certified coders continues to outpace supply, with specialized certifications creating additional hiring challenges.
High Turnover Drivers: Remote work burnout, increasing specialization needs, job stress, and competitive salary demands drive turnover rates that disrupt coding quality and consistency. Each coder’s departure represents lost institutional knowledge and introduces training lag for replacements.
Experience vs. Productivity Paradox: Research reveals that coders with more than 20 years of experience review 44 fewer charts, code 63 fewer charts, and appeal 8 fewer denials than the most productive coders, suggesting potential workflow inefficiencies or outdated practices among very experienced staff [7].
The Complexity Explosion
ICD-10-CM implementation represented the most significant coding complexity increase in healthcare history:
From 14,000 to 70,000+ Codes: The transition from ICD-9 to ICD-10 expanded the diagnosis code set from approximately 14,000 codes to more than 70,000 codes, requiring unprecedented coder education and creating ongoing challenges for specialty-specific coding [4].
Specificity Requirements: ICD-10 demands granular specificity (laterality, encounter type, clinical detail) that many physicians don't document routinely, creating gaps between clinical notes and coding requirements [4].
Annual Updates: CPT, ICD-10-CM, and HCPCS codes undergo annual revisions, with quarterly updates for certain code sets, requiring continuous education that many organizations fail to provide systematically.
The Documentation Disconnect
79% of Improper Payments: The Centers for Medicare & Medicaid Services reports that 79.11% of Medicaid improper payments result from insufficient documentation rather than intentional fraud, highlighting the fundamental disconnect between clinical documentation practices and coding requirements [6].
Table 4: Improper Payment Root Cause Analysis
69% Diagnosis Support Failure Rate: Recent Medicare Advantage audits revealed a 69% diagnosis support failure rate, where diagnoses submitted for risk adjustment lack adequate support in medical records [5]. This isn't fraud; it's documentation failure.
Physician-Coder Communication Gaps: Limited resources for Health Information Management departments result in coding quality suffering due to incomplete chart documentation, lack of communication with physicians, and time constraints that prevent thorough review and query processes [3].
The Education Gap
One-Time Training Fallacy: Many organizations provide initial coding training during onboarding but fail to implement ongoing education programs that address annual code updates, specialty-specific requirements, and emerging denial patterns.
Specialty-Specific Knowledge Deficits: General medical coders lack the specialty-specific knowledge required for complex areas like behavioral health (20-40% error rates), orthopedics (modifier-critical coding), and oncology (disease status and treatment intent documentation) [3].
Lack of Feedback Loops: Without systematic audit programs and individual coder feedback, errors perpetuate, and accuracy never improves beyond baseline training levels.
HOM's 90-Day Improvement Framework: The 3-Pillar Method
Organizations that achieve sustained coding accuracy excellence don't rely on technology alone. They implement HOM's suggested 3-Pillar Framework that has consistently delivered up to 99% coding accuracy across diverse specialties and practice sizes.
The framework operates on a simple principle: education before automation, process before technology, sustainability before scale. When implemented systematically over 90 days, this approach creates measurable accuracy improvements and revenue recovery that compounds over time.
What makes HOM's approach different: While many in the industry implement generic coding training or expensive technology solutions, the 3-Pillar Framework complements generic training with specialty-specific education, individualized audit feedback, and customized reference tools in a structured 90-day methodology that addresses root causes rather than symptoms.
Table 5: HOM vs. Common Industry Approach — Coding Accuracy Approaches

Phase 1: Assessment and Baseline Establishment (Days 1-30)
Week 1-2: Comprehensive Documentation Audit
The foundation of any accuracy improvement program begins with understanding current performance. This isn't a random sample review; it's a comprehensive analysis designed to identify specific error patterns, coder-specific challenges, and specialty-related gaps.
Assessment Components:
- Complete review of current documentation practices across all specialties and service types
- Analysis of coding accuracy and error rates by coder, specialty, and payer
- Identification of specific improvement opportunities, including modifier errors, specificity gaps, and E/M level miscoding
- Establishment of baseline performance metrics for progress measurement
Based on industry research: Organizations conducting comprehensive baseline audits identify primary diagnosis error rates of 26-32% and secondary diagnosis error rates of 9.9-10% in hospital settings, with physician practice error rates typically ranging from 15-25% depending on specialty complexity [3].
Week 3-4: Error Pattern Analysis and Education Planning
Raw audit data becomes actionable when analyzed for patterns. This phase categorizes errors by type (modifier errors, downcoding, unbundling, specificity gaps), frequency, financial impact, and root cause.
Analysis Focus:
- Specialty-specific error patterns requiring targeted education
- Coder-specific knowledge gaps indicating individual coaching needs
- Documentation deficiencies requiring physician education and query process improvement
- High-value opportunities where small accuracy improvements yield substantial revenue recovery
Phase 2: The 3-Pillar Implementation (Days 31-60)
This is where HOM's methodology delivers breakthrough results. The systematic combination of these three pillars, implemented in sequence, creates synergistic effects that dramatically outperform generic training or technology-only approaches.
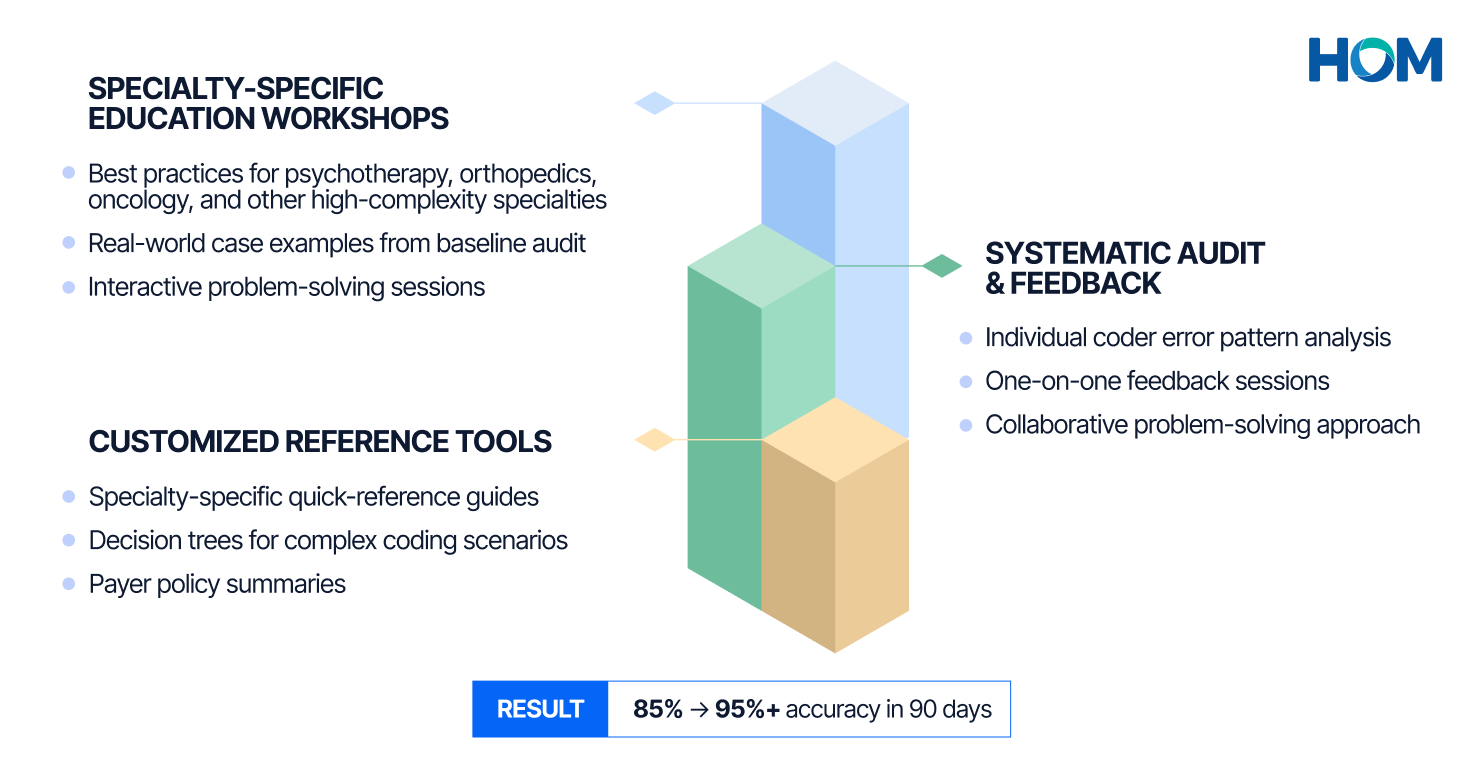
Pillar 1: Specialty-Specific Education Workshops
The cornerstone of sustainable accuracy improvement is education that addresses specialty-specific coding challenges. While generic coding training provides essential foundational knowledge for smaller organizations, specialty-specific training adds the nuanced expertise required for high-complexity medical specialties.
Workshop Design Principles:
- Best Practice Education: Focus on specialty-specific best practices, including modifier usage and code selection based on service characteristics
- Real-World Application: Use actual examples from baseline audit findings to demonstrate correct vs. incorrect coding, making education immediately relevant to daily work
- Interactive Problem-Solving: Case-based learning where coders work through scenarios, make coding decisions, and receive immediate feedback
- Documentation Requirements: Clear explanation of what documentation elements support specific codes, helping coders understand the 'why' behind coding rules
Research Foundation: Studies demonstrate that curriculum-based training programs improve coding accuracy by 15 percentage points [3]. Additional research shows physician-coder collaboration mechanisms increase accuracy from 78.9% to 87.1% [3].
Pillar 2: Systematic Audit and Feedback
Education alone doesn't change behavior. Systematic feedback loops that show individual coders their error patterns create accountability and reinforce learning.
Audit and Feedback Components:
- Sample Audits: Review of past billing cases to identify coding inconsistencies and error patterns specific to each coder's work
- Individual Feedback: One-on-one sessions providing clear feedback and guidelines to address identified issues, creating personalized improvement plans
- Error Categorization: Classification of errors by severity (compliance risk vs. revenue impact vs. minor technical errors) helps prioritize correction efforts
- Collaborative Problem-Solving: Rather than punitive feedback, the approach focuses on understanding why errors occurred and what support coders need to prevent recurrence
Pillar 3: Customized Reference Tools and Job Aids
Coders can't memorize every specialty-specific guideline, payer policy, and modifier application rule. Accessible reference tools that summarize key considerations create sustained accuracy after formal training ends.
Reference Guide Development:
- Specialty-Specific Focus: Customized coding reference guides summarizing key considerations for modifier usage and code selection based on common scenarios encountered in daily coding work
- Quick-Reference Format: Single-page guides, decision trees, and flowcharts that coders can access during coding to verify correct application of complex rules
- Payer-Specific Requirements: Documentation of payer-specific policies that differ from standard coding guidelines, preventing denials due to commercial payer variations
- Update Mechanisms: Clear processes for updating reference materials when annual coding changes take effect or new payer policies emerge
Phase 3: Optimization and Sustainability (Days 61-90)
The final phase ensures accuracy improvements become embedded in daily operations rather than temporary changes that fade after the improvement project ends.
Sustainability Mechanisms:
- Ongoing Quality Audits: Regular sampling of coded claims to identify emerging error patterns before they become systemic problems
- Continuous Education: Scheduled training on quarterly code updates, new payer policies, and denial trends identified through monitoring
- Peer Review Processes: Collaborative review sessions where coders discuss challenging cases and share specialty-specific knowledge
- Performance Dashboards: Real-time visibility into coding accuracy, denial rates, and revenue cycle metrics that demonstrate ongoing improvement and identify regression risks
- Coder Recognition: Celebration of accuracy improvements and recognition of coders who achieve excellence, creating positive reinforcement and team accountability
Proven Results: The Psychotherapy Clinic Success Story
The Challenge
A psychotherapy clinic experienced lower-than-expected revenue despite high patient volumes and positive clinical outcomes. Initial investigation revealed the problem wasn't lack of patients or poor-quality care—it was coding accuracy.
Baseline audit findings identified 85% coding accuracy, meaning 15% of claims contained errors that impacted reimbursement. The financial impact was substantial: the clinic was leaving significant revenue uncaptured through two primary error categories:
Downcoding/Undercoding: Services were billed at lower levels than documentation supported, directly reducing per-claim reimbursement.
Missed Modifier(s): Required modifiers weren't appended to codes, resulting in payer denials or bundled payment reductions.
For context, behavioral health coding presents unique challenges. Mental health ICD-10 codes show 20-40% error rates industry-wide due to overlapping symptoms, comorbidity complexity, and subjective clinical assessments [3].
The 3-Pillar Solution
Rather than implementing expensive technology solutions or expanding coding staff, HOM applied a 3-Pillar Framework with systematic education and process improvement:
Pillar 1: Coding Education Workshop
HOM designed and delivered a comprehensive education workshop focused specifically on psychotherapy and family therapy billing requirements. The workshop also focused on appending modifiers and selecting the most accurate CPT code for the therapy session, including duration, setting, and complexity.
Pillar 2: Audit and Feedback Process
HOM conducted systematic audits of the clinic's past billing cases to identify coding inconsistencies and provided feedback and clear guidelines to the coders to address these issues. Individual sessions helped each coder understand their specific error patterns and how to correct them going forward.
Pillar 3: Customized Coding Reference Guide
HOM developed a customized reference guide for the client, summarizing key considerations for modifier usage and CPT code selection based on common psychotherapy scenarios. This created an accessible resource that outlasted the formal training period.
The Results: 90-Day Transformation
The combination of targeted education, systematic feedback, and accessible reference tools delivered measurable results in just three months:
Table 6: Psychotherapy Clinic—Before/After Results
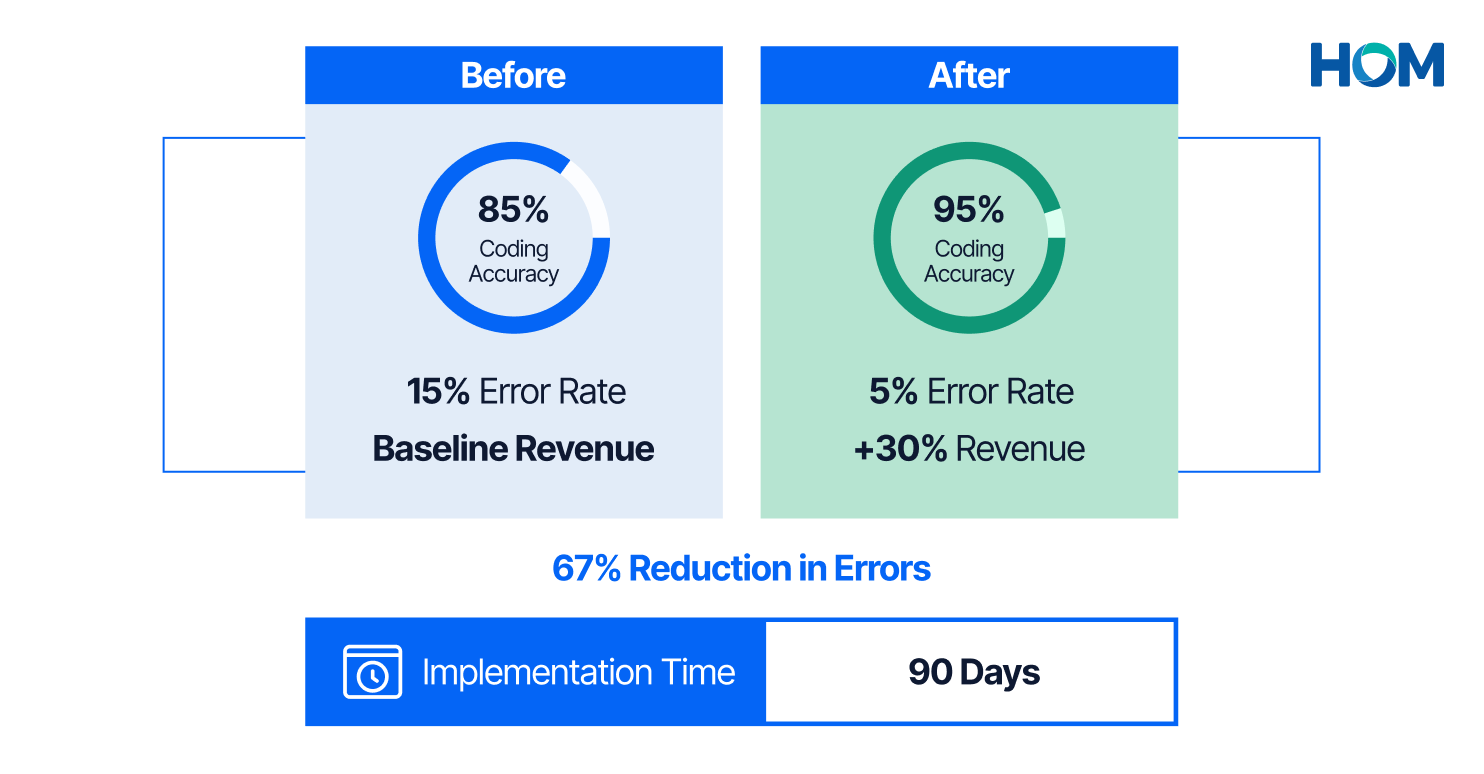
KEY INSIGHT: 67% reduction in errors translated to 30% revenue increase from the same patient volume
95% Coding Accuracy (up from 85% baseline)
The clinic achieved a 10-percentage-point improvement in coding accuracy, reaching the industry benchmark of 95%. This means that for every 100 claims coded, the number of errors dropped from 15 to 5—a 67% reduction in error rate.
Context from Research: This improvement aligns with published studies showing curriculum-based coding education can improve accuracy by 15 percentage points [3]. The psychotherapy clinic's 10-point improvement in 90 days represents accelerated results attributable to the focused, specialty-specific approach.
30% Revenue Increase
By correcting downcoding errors and ensuring proper modifier application, the clinic captured 30% more revenue from the same patient volume and service mix. This wasn't about seeing more patients or changing clinical practice—it was about getting paid appropriately for the services already being delivered.
Financial Impact: For a small-to-medium psychotherapy practice experiencing 10-30% revenue loss due to coding inaccuracies (consistent with industry data [1]), correcting these errors through a 10-percentage-point accuracy improvement would yield 25-35% revenue recovery. The clinic's 30% increase falls squarely within this expected range.
3-Month Implementation Timeline
Perhaps most significantly, these results were achieved in 90 days—not the 12-24 month timelines typical of technology implementation projects. The rapid improvement reflects the power of focused education and process improvement over complex system changes.
Key Success Factors
The psychotherapy clinic case study demonstrates several critical success factors for coding accuracy improvement:
- Specialty-Specific Focus: While essential, only generic coding training wouldn't have addressed the behavioral health-specific challenges. The targeted workshop content directly tackled the clinic's actual error patterns.
- Education Before Technology: The clinic achieved 95% accuracy and 30% revenue increase without implementing CAC software or other expensive technology solutions.
- Feedback Loops Matter: Individualized coder feedback ensured that each person understood their specific errors and how to correct them.
- Reference Tools Enable Sustainability: The customized reference guide created a resource that outlasted the formal training period.
- Measurement Drives Improvement: Establishing baseline metrics (85% accuracy) and tracking progress enabled clear demonstration of ROI.
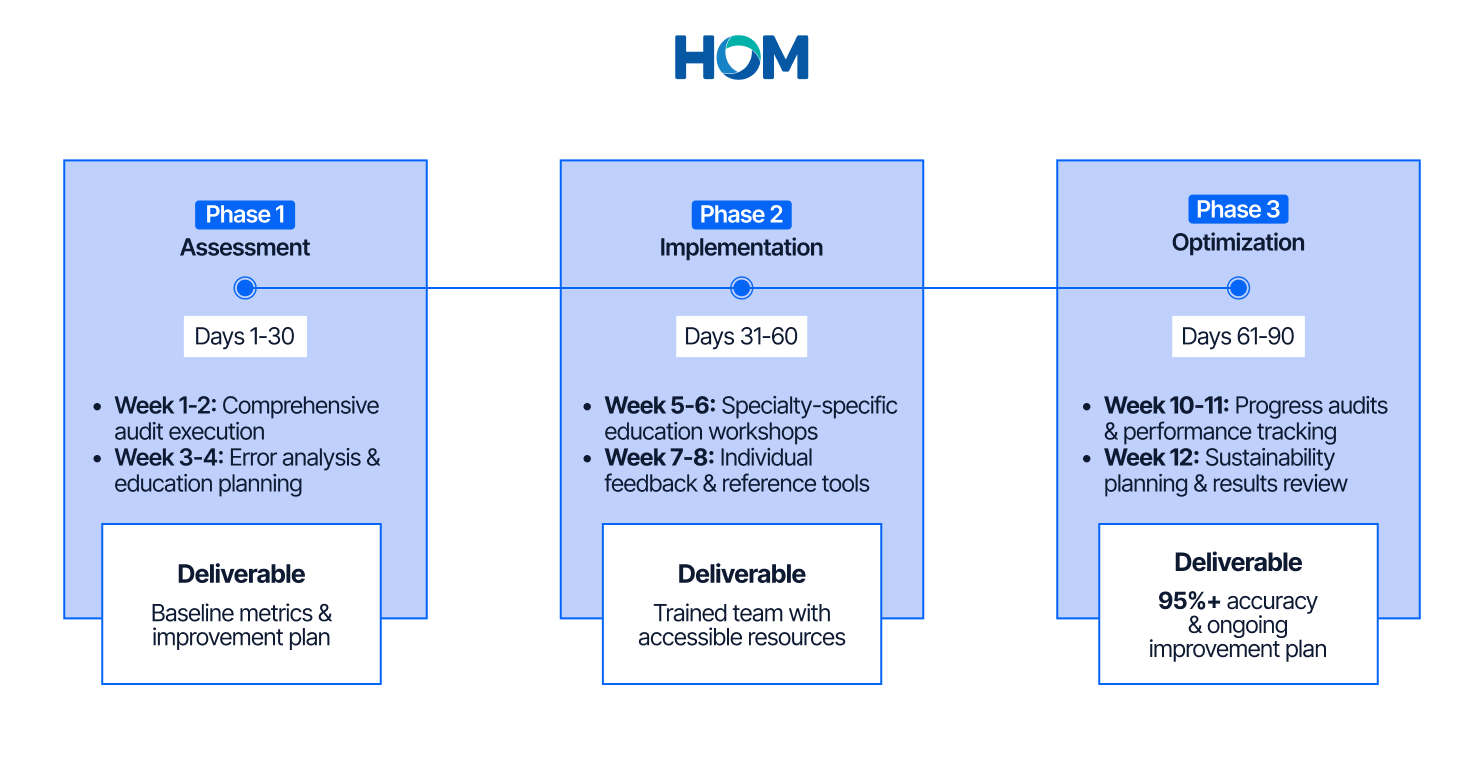
Implementation Roadmap: Your 90-Day Action Plan
Transforming coding accuracy from a compliance concern into a revenue driver requires systematic implementation. This roadmap provides week-by-week guidance for coding managers and medical directors ready to launch improvement initiatives.
Pre-Implementation: Week 0 (Preparation Phase)
Stakeholder Alignment:
- Secure executive sponsorship and budget authorization for audit, education, and consulting support
- Align with revenue cycle leadership on success metrics and reporting requirements
- Communicate improvement initiative to coding team, emphasizing education focus
- Establish project governance, including decision-making authority and progress review cadence
Baseline Data Collection:
- Identify key performance metrics to track: coding accuracy rate, denial rate by reason code, clean claim ratio, days in A/R
- Pull 3-6 months of historical performance data to establish baseline trends
- Document current coding education programs, reference resources, and quality audit processes
Phase 1: Assessment and Baseline (Days 1-30)
Week 1-2: Comprehensive Audit Execution
Day 1-3: Define audit scope, including specialties, service types, payers, and sample size. For most practices, 75-100 charts per specialty provide adequate error pattern identification.
Day 4-12: Conduct line-by-line review of selected claims, comparing coded diagnoses and procedures against documentation in medical records. Calculate baseline accuracy rates overall and by error category.
Week 3-4: Error Analysis and Planning
Day 13-27: Categorize errors by type, financial impact, root cause, and coder-specific patterns. Develop specialty-specific education curriculum addressing identified error patterns.
Day 28-30: Create measurement framework to track accuracy improvement, denial rate reduction, and revenue recovery. Schedule workshops during protected time.
Phase 2: Education and Improvement (Days 31-60)
Week 5-6: Education Workshop Delivery
Day 31-42: Conduct specialty-specific coding education workshops focusing on common error patterns identified in baseline audit, best practices for code selection, modifier application requirements, and documentation elements required to support accurate coding.
Week 7-8: Audit Feedback and Reference Tools
Day 43-49: Conduct one-on-one feedback sessions with each coder reviewing their specific audit findings. Document coder-specific education needs requiring additional support.
Day 50-60: Build customized coding reference guides including modifier usage flowcharts, code selection quick-reference tables, common scenario examples, and payer policy summaries. Distribute tools and train coders on integration into daily workflows.
Phase 3: Optimization and Sustainability (Days 61-90)
Week 10-11: Progress Monitoring
Day 61-77: Conduct post-education accuracy audits using the same methodology as baseline. Track overall accuracy improvement (target: 10+ percentage point increase), error rate by category, denial rates, and coder confidence.
Week 12: Sustainability Planning
Day 78-87: Develop ongoing education plan, including quarterly training on annual code updates, monthly coding team meetings, new coder onboarding curriculum, and continuing education requirements.
Day 88-90: Conduct final 90-day results review with stakeholders. Document accuracy improvement achieved (target: 85% → 95% or better), calculate revenue recovery (target: 20-30% increase), and establish Year 2 improvement roadmap.
Table 7: 90-Day Implementation Timeline Summary
Success Metrics and KPIs
Clinical Documentation Quality Metrics:
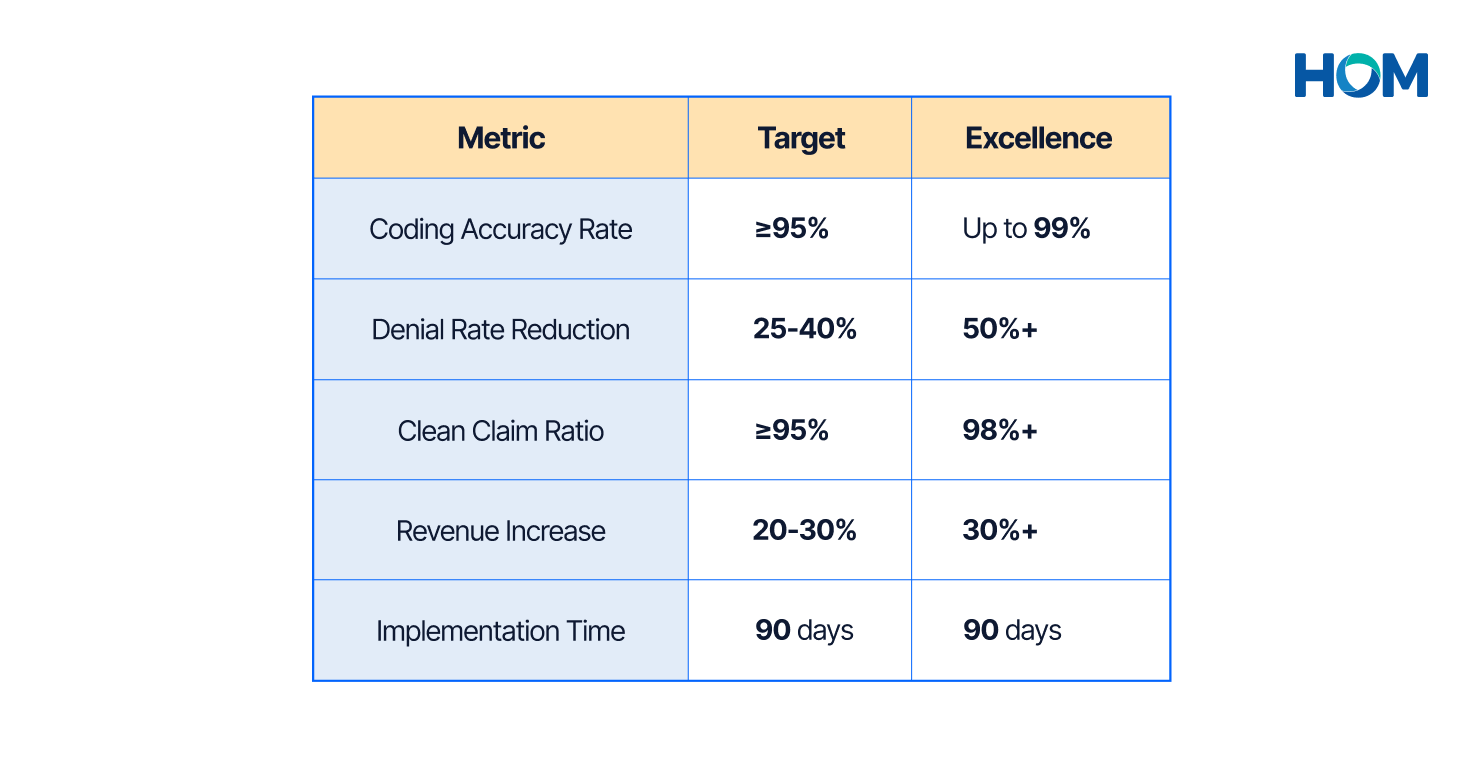
- Coding Accuracy Rate: Target ≥95% to meet industry benchmark, with up to 99% as excellence standard
- Error Rate by Category: Track modifier errors, specificity gaps, downcoding separately
- Documentation Query Rate: Monitor frequency of coder-to-physician queries, with decreasing rate indicating improved documentation
Financial Performance Indicators:
- Revenue Per Claim: Increase of 15-30% expected as downcoding is corrected
- Denial Rate: Target 25-40% reduction in coding-related denials
- Clean Claim Ratio: Target ≥95% first-pass acceptance rate
- Days in A/R: Decrease of 10-15 days expected as clean claim ratio improves
Table 8: Success Metrics Dashboard
Conclusion and Next Steps
Medical coding accuracy isn't just a compliance metric—it's the foundation of financial performance in value-based care. Organizations achieving up to 99% accuracy don't get there by accident. They implement the systematic 3-Pillar Framework suggested by HOM, combining specialty-specific education, individualized feedback, and sustainable quality processes.
The data proves the ROI: Converting 85% accuracy to 95% accuracy in 90 days drives 30% revenue increases without seeing additional patients or expanding services. These aren't theoretical projections; they're documented results from real-world implementations.
Key Success Factors:
- Education Must Be Specialty-Specific: Generic medical coding training fails because it doesn't address actual scenarios coders encounter daily
- Feedback Drives Behavior Change: Coders need to see their specific error patterns with clear explanation of correct approaches
- Reference Tools Enable Sustainability: Accessible job aids ensure learned concepts transfer to daily coding decisions beyond formal training
- Measurement Validates Progress: Baseline metrics, interim tracking, and final outcomes documentation demonstrate ROI
- Continuous Improvement Culture Matters: Sustainable excellence requires ongoing education, regular audits, and leadership commitment
The Strategic Advantage
While competitors struggle with 80% accuracy and rising denial rates, organizations implementing HOM's systematic framework capture 15-20% more revenue from existing patient volumes. In a $10 million practice, that's $1.5-2 million in additional annual revenue—not from seeing more patients, but from getting paid appropriately for services already delivered.
As Medicare Advantage audit activity intensifies (69% diagnosis support failure rates in recent audits [5]) and OIG enforcement escalates ($14.6 billion in 2025 fraud takedown [11]), coding accuracy becomes not just a revenue opportunity but a compliance imperative.
Next Steps for Coding Managers and Medical Directors
- Conduct Baseline Assessment: Evaluate current coding accuracy and identify high-priority improvement opportunities
- Quantify Financial Opportunity: Calculate your organization's potential revenue recovery based on current error rates and claim volume
- Build Business Case: Document current accuracy metrics, denial rates, and revenue leakage to secure executive sponsorship
- Identify Quick Wins: Focus initial efforts on high-volume, high-error-rate specialties where rapid improvement delivers maximum ROI
Ready to Transform Your Coding Accuracy?
The framework is proven. The ROI is documented. The timeline is achievable. Organizations that commit to systematic coding accuracy improvement position themselves for financial success in an increasingly complex reimbursement environment.
The question isn't whether coding accuracy improvement delivers value—the data proves it does. The question is whether you'll implement it before your competitors do.
References and Sources
#
References
Public Link
1
Simbo.AI "Financial Impact of Medical Coding Errors" (2024)
2
Becker's Payer Issues and OS Healthcare 2024 data (Pub. May 2025)
https://www.beckerspayer.com/payer/claims-denial-rates-up-prior-auth-denials-down-in-2024-report/
3
NIH (PMC) "Medical Coding Accuracy and Clinical Documentation Quality"
https://pmc.ncbi.nlm.nih.gov/articles/PMC9898522/
4
NCHS "ICD-10-CM Implementation Impact Study" (2024) - A commonly cited peer-reviewed paper
https://pmc.ncbi.nlm.nih.gov/articles/PMC4142514/
5
OIG "Medicare Advantage Compliance Audit Results" (2024)
https://oig.hhs.gov/reports/all/2024/medicare-advantage-compliance-audit-of-specific-diagnosis-codes-that-independent-health-association-inc-contract-h3362-submitted-to-cms/ and https://oig.hhs.gov/reports/all/2024/medicare-advantage-compliance-audit-of-specific-diagnosis-codes-that-humana-health-plan-inc-contract-h2649-submitted-to-cms/
6
CMS "Fiscal Year 2024 Improper Payments Fact Sheet" (Nov 2024)
https://www.cms.gov/newsroom/fact-sheets/fiscal-year-2024-improper-payments-fact-sheet
7
Illinois State Board of Education "Medical Coder Productivity Benchmarks"
https://www.isbe.net/CTEDocuments/HST-630199.pdf
8
Oncology News Central 2025 Report
9
AAPC "Medical Coding Workforce Report" (2025) - Official AAPC 2025 workforce-related publication page
https://www.aapc.com/resources/medical-coding-salary-survey
10
IJISRT "AI Applications in Medical Coding Accuracy"
https://www.ijisrt.com/assets/upload/files/IJISRT25SEP1014.pdf
11
Miller Shah LLP "HHS-OIG Healthcare Fraud 2025 Report" (Spring 2025) - Direct underlying OIG report
https://millershah.com/blog/hhs-oig-healthcare-fraud-2025-report/ and https://oig.hhs.gov/reports/all/2025/spring-2025-semiannual-report-to-congress/
About HOM
HOM delivers tech-powered revenue cycle management for human-centric patient care. For close to 8 years, we've partnered with US healthcare providers to optimize operations through our 3-Pillar Framework and comprehensive RCM services.
Our proven approach has helped organizations achieve up to 99% coding accuracy, 95% denial recovery rates, and 48-72 hour turnaround times across 15+ medical specialties.
Ready to optimize your medical coding accuracy?
Contact us for a comprehensive assessment of your organization's coding performance and revenue recovery opportunities.
Website: homrcm.com
Email: partnerships@homrcm.com
Bring a change to your Healthcare Operations
A partnership with HOM gives you an inherent:
Connect with our experts for a quick analysis and possibilities.















